Case Study: Reversing Adult Scoliosis with XLIF

When many people think of scoliosis, they often think of younger children. After all, many of us probably underwent a scoliosis screening during our grade school years. Scoliosis, however, doesn’t just affect children and adolescents.
Adult-onset scoliosis, sometimes known as degenerative scoliosis, can be a part of the aging process. Unlike childhood scoliosis, this is a gradual deformity affecting the strength and structure of the spine. As a result, the spine can start to curve to the left (levoscoliosis) or the right (dextroscoliosis). This generally occurs in the lower back.
Meet the Patient
The patient was a 76-year old retired attorney who lived a fairly active life. In fact, he often enjoyed tango dancing in his free time. The man sought help for severe lower back pain and stiffness. In addition, he struggled with left leg weakness which made it difficult for him to walk.
During the physical examination, Dr. Daveed Frazier noted severe weakness in the patient’s legs. The exam also revealed an obvious curve in the lumbar spine or lower back.
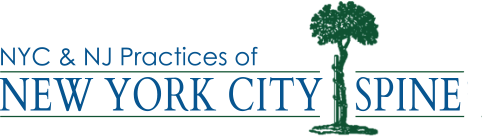
Dr. Frazier ordered AP x-rays (meaning, the x-ray beams pass from the front to back of the body) and lateral x-rays (taken from the side of the patient). The imaging revealed lumbar spondylolisthesis, which occurs when a vertebra slips over the one beneath it. In addition, an abnormal curve in the lower back was confirmed. Dr. Frazier also noted collapsed discs in the lumbar region (L1-L5).
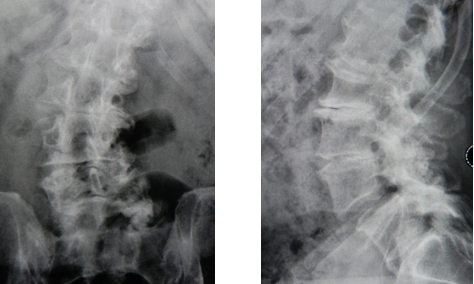
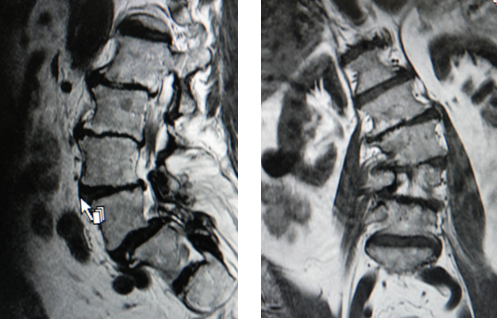
To take a better look at the area, Dr. Frazier ordered an MRI. The MRI imaging showed that the patient was suffering from osteoarthritis, scoliosis, spinal stenosis, and degenerative spondylolisthesis.
As a result, Dr. Frazier diagnosed the man with severe lumbar spondylolisthesis and lumbar spinal stenosis. Further diagnostic imaging revealed hypertrophic facets—enlargement and degeneration of the small joints along the spine which provide for lumbar stability and flexibility.
Understanding Degenerative Scoliosis
Degenerative scoliosis refers to a curve in the lower back spine. The curve forms a slight “C” shape. It occurs when there is instability in the spine, usually because of osteoarthritis or degenerative disc disease.
The spine serves an important role in protecting the spinal cord and supporting the body’s movements. The intervertebral discs between each vertebra act as cushions to absorb the shocks of our everyday activities. In addition, the facet joints, located at the back of the spine, provide flexibility during movements.
As we age, these important parts of the spinal column start to deteriorate as they continue to support our everyday activities. Some people, for a variety of reasons, experience this degeneration quicker than normal. As a result, the facet joints become less stable and the discs dry out and lose shape. This causes the vertebrae to gradually shift, causing abnormal curves to appear in the spine.
As the spinal column changes shape, it creates a narrowing of the spinal canal—the area that houses the spinal cord. Known as lumbar spinal stenosis, this narrowing can apply pressure to the spinal cord or nerve roots, generating pain and muscle weakness. At first, pain may be sharp or shock-like. It can radiate down the buttocks and into the leg—a condition known as sciatica.
Sometimes the nerves can become so damaged that they stop functioning properly. This may lead to very serious medical conditions depending on the nerves affected, like paralysis or loss of bodily functions.
Treating Adult-Onset Scoliosis
When the spine becomes unstable due to scoliosis and other complications, sometimes spinal fusion surgery is necessary. Spinal fusion surgery involves removing diseased discs and replacing them with bone grafts. Over time, these bone grafts allow the vertebrae to grow together as one bone. This procedure helps to minimize excessive movement of the spine and relieves pressure on the spinal cord or nerve roots.
There are a few different ways this type of surgery is approached. Depending on a patient’s condition, the surgeon may want to complete a fusion from the front of the body (ALIF), the back (PLIF), or through the side (XLIF). Each type of surgery has its benefits and risks. The decision is ultimately up to you and your doctor based on your condition, overall health, and desired outcomes.
The XLIF Procedure
In the case of this patient, Dr. Frazier chose a lateral lumbar interbody fusion (XLIF) approach to spinal fusion. This minimally invasive spine surgery involves treating the spinal condition by entering the side of the body (lateral entry). Unlike other approaches, it doesn’t require the surgeon to cut through muscles or move important organs or blood vessels. As a result, there is less damage to the body during surgery. While this approach may not be appropriate for everyone, Dr. Frazier believed this patient would benefit from an XLIF surgery.
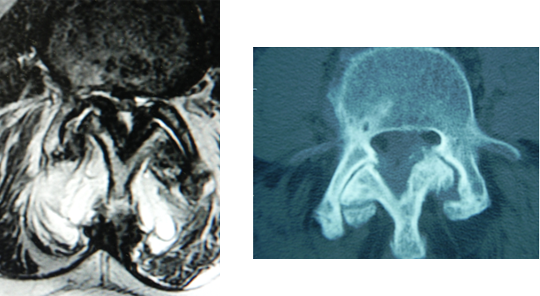
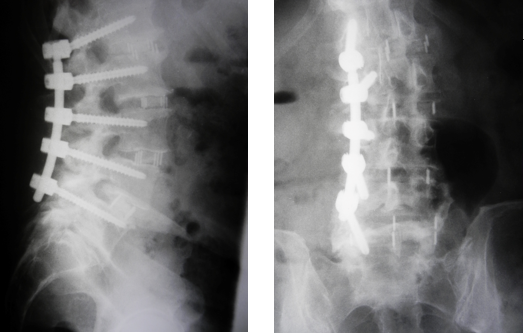
While under anesthesia, Dr. Frazier gained access to the patient’s spine using small incisions at the side of the body. Since it was a minimally invasive surgery, Dr. Frazier used x-ray fluoroscopic imaging to obtain a better look at the area during the procedure. Using the fluoroscope and tiny instruments, he removed any damaged tissues. He placed bone grafts and immobilized the joints with pedicle screws. In addition to the screws, Dr. Frazier used interbody cages to give added stability to the spine and facilitate quicker healing. These cages are titanium cylinders placed in the disc space to allow the bone grafts to mature more quickly.
The surgery took about two and a half hours to complete. Postoperative X-rays showed the correction of the scoliotic deformity. In addition, the disc heights were restored, allowing more room for the nerve roots.
Minimally Invasive Spine Surgery (MISS) in Action
Minimally invasive spine surgery (MISS) is designed to help patients recover quicker with less pain after surgery. In the case of this XLIF surgery, the patient experienced several benefits and positive outcomes. These included:
- Less blood loss: Open surgeries can lead to a lot of blood loss. During this minimally invasive surgery, the patient only lost 20 CCs of blood. This is less than two tablespoons of blood.
- Less damage to surrounding tissues: By using a lateral entry, Dr. Frazier did not have to complete any muscle stripping to gain access to the area. Less soft tissue damage during surgery means less postoperative pain.
- Quicker recovery times: For elderly patients with multilevel spinal conditions, MISS can significantly reduce recovery times compared to open back surgery. This patient was able to return home after two days. In addition, he had improved function, decreased weakness, and better posture after leaving the hospital.
- Returning to normal activities quicker: Just five weeks after surgery, the patient went on a trip to Argentina to celebrate his recovery. In addition, this 76-year-old improved his flexibility enough so that he could touch his toes from a standing position.
Are you interested in learning more about minimally invasive spine surgery? Dr. Daveed Frazier is a Harvard-trained, board-certified orthopedic spine surgeon. In addition, he was recognized by New York Times Magazine as a “New York Super Doctor” on two separate occasions. In his over 20 years of experience, he has helped countless individuals who suffer from a variety of spinal conditions. Find out how he can help you today!