What is Ankylosing Spondylitis or Bamboo Spine?
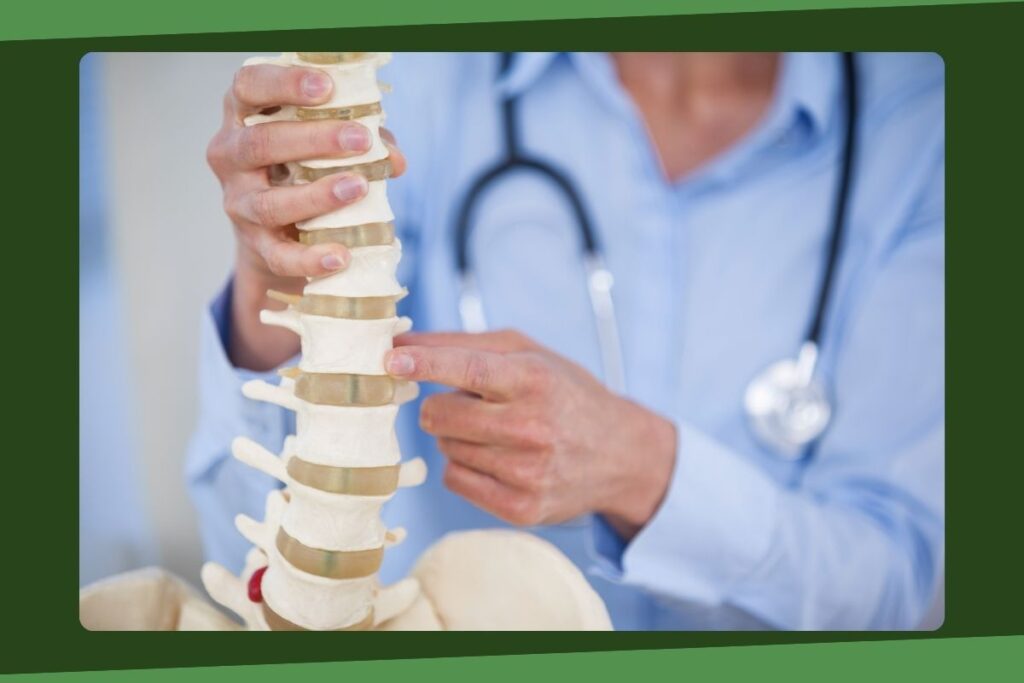
Ankylosing Spondylitis (AS) is a chronic inflammatory disease affecting multiple body systems. Usually, AS attacks the spine and sacroiliac joints, but it can also adversely affect other joints and organs. AS leads to spine stiffening and inflammation in the joints. In rare cases, AS may even cause the spinal vertebrae to fuse. When vertebrae fuse entirely, this is known as ankylosis.
More accurately, AS causes the exterior fibers of the annulus fibrosus in our intervertebral discs to ossify, which leads to a spine that appears fused between each vertebra. Indeed, this is where the term “bamboo spine” comes from. The spine develops a bamboo-like appearance because of the joining of adjacent discs.
Causes of Ankylosing Spondylitis (AS)
The medical community widely believes that ankylosing spondylitis develops because of a genetic predisposition. The vast majority of AS patients were born with the gene HLA-B27. In recent years, the medical community has developed blood tests to screen for this gene. In doing so, our understanding of the gene’s association with this condition has improved dramatically.
Of course, having this gene isn’t necessarily a sentence for developing AS. Studies show that additional factors—likely environmental—must be present for the disease to manifest. The reason for this belief is because of the way the numbers stack up. In the United States, 7% of people have the gene in question. That being said, only 1% of the population develops AS. So, while the gene is commonly found in patients with the condition, it is certainly not the only factor at play.
Medical experts also suggest that genes ARTS1 and IL23R are responsible for the manifestation of AS. This belief exists mainly because these genes affect our body’s immune system. The medical community accepts this as a notable risk factor for developing the disease.
How the disease occurs and spreads to different body areas is still poorly understood. It is a highly complex ordeal, as every individual seems to have their manifestation of the disease. Perhaps the disease came into play because of the body’s immune functions, or maybe it spawned from some bacterial infection. The main point is that the disease is only understood in bits and pieces. The medical community is actively researching the disease to understand how it works and how to treat it best.
Ankylosing Spondylitis (AS) Signs & Symptoms
The symptoms of AS are associated with inflammation and arthritis in several body parts, including the spine, joints, and specific organs. With active inflammation, fatigue often accompanies the symptoms of AS. Spinal inflammation causes stiffness and pain in the lumbar region, the cervical area, and the upper buttocks. Of course, these symptoms may also affect other parts of the spine. Usually, these symptoms are progressive, meaning they only worsen with time, ultimately leading to a loss in overall range of motion. Additionally, the onset of these symptoms tends to be rapid and intense.
A complete bony fusion between vertebrae may occur in severe cases involving the spine. When this happens, the pain disappears, but at the steep price of losing all spinal mobility. This new bamboo-like spine is quite brittle and vulnerable to fractures via trauma, such as with contact sports activities. Usually, the pain manifests suddenly when a spinal fracture such as this occurs.
Both spondylitis and ankylosis cause forward spinal curvature of the thoracic region, which limits the patient’s ability to breathe properly. Additionally, these problems affect where the ribs attach to the upper thoracic spine, further decreasing the patient’s lung capacity. As you can see, breathing becomes a major problem with AS.
Other areas affected by the condition are the heart, eyes, and kidneys. Some patients with AS may develop iritis (inflammation of the iris). Iritis is easily identifiable by the redness and pain of the affected eye, which is exacerbated when the patient looks at bright lights. AS may also cause scarring in specific tissues of the heart, which in turn slows down the patient’s heart rate. Lastly, protein deposits (amyloid) in the kidneys from AS may lead to kidney failure in patients with the disease.
Ankylosing Spondylitis (AS) Diagnosis & Treatment
Usually, a doctor diagnoses AS through a physical exam. The doctor asks the patient to bend into different orientations to examine the state of the spine’s motion range. After getting a rough idea of where to look, the doctor will try to put pressure on specific areas of the pelvis and/or legs to find affected bodily regions.
Of course, doctors will also use imaging and lab tests as they see fit. For example, an MRI will help by showcasing all the details of the body’s bones and soft tissues. Although more expensive, MRIs typically show signs of AS earlier than normal X-rays do.
Specific blood tests are also performed by doctors to check for symptoms such as inflammation. However, this inflammation could theoretically come from anywhere—not just AS. It’s more likely that the patient’s blood will be tested for the HLA-B27 gene, even though most of these gene carriers don’t have AS.
Non-surgical Treatments for AS
Doctors resort to a slew of treatments when treating patients with AS. One is commonly giving their patients NSAIDs (such as Naproxen) to help with inflammation. These drugs may also help with the pain and stiffness that come naturally with inflammation.
Sometimes, however, NSAIDs are not enough. In such cases, your doctor may prescribe a biologic medication, such as a TNF blocker. These medications target cell proteins in the body that lead to inflammation. TNF blockers also help with stiffness, pain, and sensitive joints. The doctor will administer this medication via an intravenous line underneath the skin.
Surgical Treatments for AS
The type of surgery your spine surgeon considers for your case will depend on many variables. Such factors include your symptoms, severity of spinal abnormalities, age, lifestyle, etc. It is not uncommon for a patient with AS to undergo more than one surgical procedure. Here are a few examples of the most common ones:
- Osteotomy: The surgeon cuts the bone to normalize angular deformities in the spine. After the doctor cuts and extracts the wedge, the bone ends are reunited so that they may heal together. Oftentimes, your doctor will resort to rods, screws, and spinal fusion to help stabilize the spine during recovery.
- Spinal Instrumentation & Fusion: These procedures focus more on maintaining stability in the spine and correcting the initial deformity. Fusion joins the bones together at the affected area so that bones may heal back together again. Rods and screws typically help with stability by holding the spine straight during this process.
- Laminectomy: Laminectomies are decompression procedures that do exactly what they sound like they do. The performing doctor decompresses the spinal canal, which relieves nerves in the affected area, thereby improving function.
Of course, these are just a few common examples. Make sure to communicate with your doctor to understand your medical avenues better.
Have you recently had a surgical procedure on your spine that didn’t quite work out? Still, feeling stiff? Is it a pain to stand upright? If so, you might want to call us at (855) 210-0899. It’s hard to live your life in chronic pain, so it never hurts to reach out to a team you can trust. Our spine surgeons will work tirelessly to ensure that you are put on a treatment plan that is tailor-made to suit your specific needs.