-
Pain Topics
- Ankylosing Spondylitis (0)
- Arthritis (5)
- Back Pain (35)
- Bulging Disc (3)
- Degenerative Disc Disease (2)
- Facet Joint Syndrome (1)
- Failed Back Surgery (1)
- Foraminal Stenosis (2)
- Herniated Disc (5)
- Kyphosis (1)
- Neck Pain (14)
- Osteoporosis (2)
- Paget's Disease (1)
- Pinched Nerve (3)
- Radiculopathy (1)
- Sciatica (5)
- Scoliosis (5)
- SI Joint Arthritis (1)
- spinal cord injury (4)
- Spinal Deformity (1)
- Spinal Fractures (3)
- Spinal Stenosis (2)
- Spinal Tumors (1)
- Spondylolisthesis (3)
- Spondylosis (2)
- Whiplash (2)
-
Treatment Topics
- ALIF (2)
- Artificial Disc Replacement (1)
- At Home Care (4)
- Chiropractic Care (3)
- Corpectomy (1)
- Diagnostic Procedures (2)
- Diet & Healthy Lifestyle (6)
- Everyday Ergonomics (2)
- Exercises & Stretches (4)
- Facet Joint Infection (1)
- Foraminotomy (2)
- Kyphoplasty (2)
- Laminectomy (2)
- Laminotomy (2)
- Massage Therapy (1)
- Microdisectomy (2)
- Minimally Invasive Spine Surgery (13)
- Nonoperative Solutions (7)
- Pain Management (6)
- Physical Therapy (2)
- PLIF (3)
- Revision Spine Surgery (2)
- Scoliosis Brace (2)
- Self-Care (7)
- Spinal Fusion (3)
- TLIF (3)
- XLIF Corpectomy (4)
-
Media & Interactive
Resolving SI Joint Arthritis from Adjacent Segment Disease
Meet the Patient
The patient was a 68-year-old male with diabetes and severe sacroiliac pain. The patient communicated with Dr. Frazier that he had extreme difficulty traversing uneven terrain, as well as difficulty sitting for prolonged periods of time.
Here are a few characteristics that the patient shared with Dr. Frazier that were relevant to reaching a diagnosis:
- Lifestyle: The patient was a white-collar banker who sat for prolonged periods of time. Sitting for long periods of time such as this is the number one risk factor for developing spinal problems down the road.
- Failed Back Surgery Syndrome: The patient reported his symptoms to Dr. Frazier after recently having undergone a spinal fusion procedure. When a procedure such as this fails, it may lead to something known as adjacent segment disease/degeneration (ASD). This causes problems in the joints above and below the affected areas that were the target of the initial procedure. Additionally, this condition may occur at any point on the spine.
- Obesity:Excessive weight means that the structures supporting the body are responsible for supporting more weight than they are “designed” to. This leads to a slew of wear-and-tear related problems, such as arthritis or slipped discs.
- Diabetes: Obesity strongly correlates with diabetes (although not all patients with diabetes are overweight). And, patients with diabetes are more likely to experience issues in the spine and adjacent areas.
Diagnosing SI Joint Arthritis
- The Physical Exam: After obtaining ample information about the patient’s history, Dr. Frazier began his search by performing a quick physical exam. During this examination, Dr. Frazier found that the patient had severe gluteal spasms and quadriceps weakness. Considering the patient’s history, this suggested SI joint arthritis resulting from adjacent segment disease.
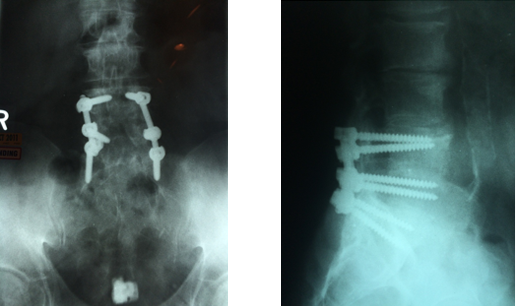
- Preoperative Imaging: Keeping this in mind, Dr. Frazier conducted AP and lateral x-rays, which showed severe SI arthritis and L3-4 adjacent segment degeneration in the setting of a prior L4-S1 decompression/fusion.
- Official Diagnosis: With x-ray confirmation, Dr. Frazier was able to determine that the patient had SI joint arthritis as a result of adjacent segment degeneration from the prior surgery.
Regarding SI Joint Arthritis
Sacroiliitis is a blanket term that medical professionals use to describe any inflammation in the sacroiliac joint. For context, the sacroiliac joint sits on either side of the lower spine (sacrum) which connects the iliac bone to the top of the hips.
Usually, sacroiliitis is found as a secondary problem to other inflammatory problems existing within the spine. As such, these conditions exist among a category that medical professionals refer to as “spondyloarthropathy.” This set of conditions includes diseases such as ankylosing spondylitis, psoriatic arthritis, and reactive arthritis. Usually, the medical community uses the terms “sacroiliitis” and “sacroiliac joint dysfunction” interchangeably, as both terms describe pain that stems from the same place (the SI joint).
That being said, there are actually two distinctions between the two:
- Sacroiliac Joint Dysfunction: This condition refers to pain in the sacroiliac joint that is triggered by abnormal motions in the joint. This may be due to either too little or too much abnormal movement. Naturally, it results in inflammation of the joint in question.
- Sacroiliitis: This term has a broader application. Anything ending in “itis” has its hand in inflammation and sacroiliitis is no different. Sacroiliitis describes inflammation of the sacroiliac joint. However, the important distinction here is that it doesn’t necessarily mean that the inflammation is caused by dysfunction.
Symptoms for sacroiliitis include:
- Fever
- Pain that manifests in the lumbar spine, legs, hips, and buttocks
- Discomfort that worsens when sitting for prolonged periods
- Aching that exacerbates when rolling over while lying down
- Stiff hips and lower back—especially so when getting out of bed or sitting for long periods of time
Of course, these are just a few general warning signs. Your symptoms may vary depending on the specifics of your case.
SI Joint Arthritis Surgery
To serve our patient, Dr. Frazier decided that the best course of action would be to perform an SI fusion with percutaneous screws and extreme lateral interbody fusion (XLIF) with a lateral plate. The procedure lasted approximately an hour and the patient only lost 20 ccs of blood.
Why Choose Minimally Invasive Spine Surgery (MISS)
Generally speaking, there are three levels of treatment: conservative, minimally invasive surgery, and traditional open surgery. Each of these tiers carries their own advantages and disadvantages. Ideally, you want to be as low on this totem pole as possible, but sometimes it is necessary to bump a patient up from conservative to minimally invasive procedures. Luckily, this is not a very big bump, as minimally invasive surgeries are just that: less invasive. These procedures involve minimal blood loss, scarring, quick recovery times, and are often performed on an outpatient basis. Basically, if you have to have surgery, this is what you want. Of course, not all conditions are treatable via minimally invasive surgery. Some cases simply require things that only traditional open surgery can provide. For more information, consult with your doctor.
The Procedure Rundown
In our example, Dr. Frazier performed an XLIF, a type of MISS. Doctors typically perform this procedure through the side of the body. Usually, doctors use XLIF to treat certain spinal conditions as well as reduce chronic leg and back pain. This is especially so if other more conservative methods have not been able to treat chronic pain.
Here is how doctors typically perform an XLIF:

- After you have fallen asleep, your doctor will position you on your side. Using x-ray guidance, your doctor will remove the affected disc and will make a small mark on the skin above the affected area.
- A small incision is made on the back. Your surgeon will place their finger through this entry point to ensure that the peritoneum (the sac that contains organs) stays protected. The surgeon will then use this access point to insert specialized instruments as necessary.
- A second incision is made on the side of the body, which instruments will also pass through in order to remove material such as herniated discs.
- Your surgeon will then make use of special instruments, known as tubular dilators, which they will insert through the muscle on the side of the affected vertebrae.
- After the surgeon places the dilators, they will then place a tissue retractor over them in order to stretch the small incisions, thus providing light and access to the disc space.
- Now that the affected disc is highly visible and easy to get to, the surgeon removes it.
- The surgeon replaces the affected disc with an implant, which he or she fills with bone graft for fusion purposes.
- Your surgeon again utilizes x-ray imaging to safely remove the instruments and close the incisions.
- At certain points during the surgery, your doctor may add extra steps if necessary. This includes adding additional structural support, such as screws, plates, or rods.
Contact Us
If you have pain in your joints—even if you do not think it requires surgery—please contact us today at (855) 210-0899. Dr. Daveed Frazier of New York City Spine always know just the right steps to take with any situation. With our expert team behind you, you can rest assured knowing that your spine is in caring and capable hands.
TAGS: SI Joint Arthritis XLIF
Explore New York City Spine

