Everything You Need to Know About Microdiscectomy

Why A Microdiscectomy?
The spine is a critical, yet oftentimes vulnerable, facet of the body. Composed of many collaborative components, the spine functions to support, mobilize, innervate, and cushion the body throughout our daily lives.
Things do not always go smoothly, however, and the spine can run into problems. One of the most commonly experienced spinal ailments is bulging or herniated discs.
Bulging & Herniated Discs
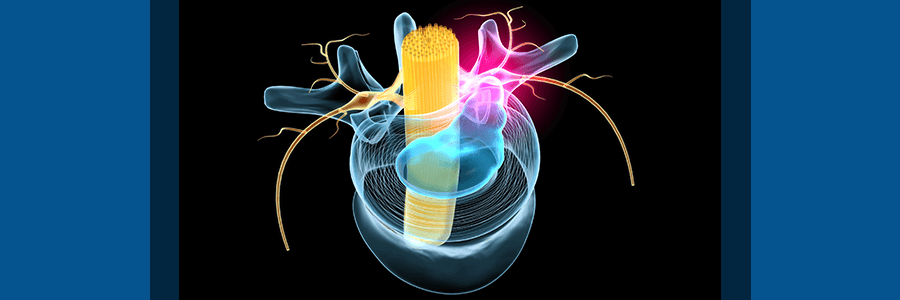
Our intervertebral discs are puck-shaped cylinders found between each of our vertebrae. Composed similarly to a jelly donut, they have a tough exterior wall filled with a gelatinous center. When healthy, these discs provide a cushiony pillow to absorb any pressure and provide a lubricating buffer between vertebral bones. When unhealthy, they can bulge or herniate, leading to debilitating nerve pain.
The difference between a bulging and herniated disc is fairly clear, however. Yet, they both can lead to pain. A bulging disc involves the protrusion of the rubbery outside of the disc from its normal location between the vertebrae. On the other hand, a disc herniation involves the cracking and breaking of the disc altogether. A herniated disc’s jelly-like interior can protrude outward from the disc, leaking into adjacent areas.
Despite their difference in details, both bulging and herniated discs can cause excruciating pain and concerning symptoms. These symptoms occur due to spinal root nerve compression. Pain, numbness, tingling, radiating discomfort that spreads into the limbs, muscular spasms, or tightness… Even immobility can result from this nerve compression.
Common Causes of Herniated Discs
The causes of Herniated Discs vary and can also depend upon the individual. Some of the most common causes include:
- Degenerative Disc Disease: This is a common condition caused by age and normal wear and tear. Degenerative Disc Disease leads to drying, thinning, and breaking of the intervertebral discs.
- Spinal Injury & Trauma: Accidents and falls can lead to spinal trauma and damaged discs.
- Osteoarthritis: Arthritis can lead to damaged discs by causing cartilage breakdown and vertebral joint inflammation.
- Spinal Tumors: The growth of tumors can encroach on intervertebral discs, leading to damage and herniation.
Despite a high rate of occurrence, a number of treatments can mitigate the painful and debilitating effects of damaged discs. Although it is often suggested that one start with conservative treatments, sometimes surgery is the best and only option for relief. One of the most successful options for herniated disc surgery lies in the minimally invasive microdiscectomy.
What is a Minimally Invasive Microdiscectomy?
A minimally invasive microdiscectomy is a state-of-the-art procedure that addresses painful herniated discs. Using specialized tools and magnifying microscopes, the surgeon uses their knowledge and skills of microsurgical techniques to deliver optimum results. Furthermore, sophisticated advances in instrumentation allow for little damage and impact to the surrounding tissues.
The procedure generally unfolds in the following steps:
- Under general anesthesia, your surgeon will begin by making a small incision in your back over the spine. This tiny incision provides your surgeon with access to the damaged intervertebral disc in the cervical, thoracic, or lumbar spine. Furthermore, this method replaces previous techniques which involved large incisions and extensive scarring.
- Using micro-instruments, the muscles, tendons, and nerves in the back will be gently pushed to the side to permit unobstructed access to the spine. This avoids the traditional incising of these tissues, which tended to result in considerable blood loss, scarring, and pain.
- The surgeon will then remove a small portion of the lamina and/or foramen to provide an optimum view and access to the damaged disc.
- Using micro-instruments, the surgeon will remove small pieces of the damaged disc to relieve pressure on the adjacent nerves.
- Muscles and other tissues will be released back to their original locations. Your surgeon will then close the small incision with a few sutures or even Steri-strips in some cases.
Following surgery, you will spend a short time in the recovery room. Clinicians will use this time to monitor your immediate recovery from the procedure and prepare you for discharge. Yes, you heard that right. Most individuals will have a microdiscectomy performed as a same-day surgery. The advent of minimally invasive technologies and techniques have provided this as well as a number of other benefits.
The Benefits of a Minimally Invasive Microdiscectomy
The benefits of minimally invasive surgery are becoming more apparent with successful results and continuous advances in technique and instrumentation. Some of the benefits of a minimally invasive microdiscectomy include:
- Small Incision Sizes: Requiring only a 1-to 2-inch incision, patients incur less scarring, less chance for infection, and a faster healing time.
- Less Damage: With no incision to the thick muscles, tendons, and ligaments of the back, the body experiences less trauma and blood loss.
- Less Pain: With smaller incisions and less trauma to the body, the patient will experience less overall pain following surgery.
- Shorter Hospital Stays & Faster Recovery Times: Most often performed as an outpatient procedure, patients can return home the same day and begin their rehabilitation process.
Exploring minimally invasive treatment options to repair a bulging or herniated disc? Dr. Frazier of NYC Spine is a Harvard-trained spine specialist, who has earned over 20 years of surgical experience in diagnosing and correcting disc deterioration!