Case Study: Surgical Treatment of Secondary Spinal Tumors

What is a Secondary Spinal Tumor?
A secondary spinal tumor occurs when cancer metastasizes (or spreads) to the spine from another area of the body. By far and away the leading cause of spine cancer, secondary tumors account for more than 90% of all spinal tumors.
But, how do these tumors spread from point A to point B in the first place? Abnormal cells can spread to the spine through the bloodstream, where they take root in our bone marrow, and multiply. Of the many cancers that can spread to the spine, lung, breast, and prostate cancers are often to blame.
Furthermore, when these metastatic tumors invade the spine, 3 main types of spinal tumors can result:
- Vertebral Column Tumors (VCT): The vast majority of spinal tumors affect the bony elements of spine. Doctors also refer to the bones of the spine as the vertebral column, because our vertebrae stack up into what resembles a pillar. In addition, 70% of all VCTs affect the thoracic level of the spine.
- Intradural-Extramedullary Tumors (IET): These tumors occur inside the protective sheath of the spinal cord (known as the dura), but outside of the true core of the spinal cord (known as the medulla). These tumors do not invade spinal nerve fibers, but may form on the nerve sheath.
- Intramedullary Tumors (IMT): In contrast, IMTs develop on actual nerve fibers, such as the spinal cord or the nerve roots that radiate out to the body. Because these tumors arise from glial cells (the “glue” that holds our nervous system together), they can be impossible to remove.
Less commonly, primary spinal tumors can arise in the spine and spread to liver, lungs, or long bones of the limbs. However, this occurs in less than 10% of all spine tumors.
Meet the Patient
The patient was a 60-year-old man with a documented history of prostate cancer. The man had been experiencing back pain for quite some time, when he suddenly lost his ability to walk. This loss of mobility had been going on for 3 days by the time that the patient was able to see a doctor. On top of this, the patient had developed urinary incontinence, a rare complication of severe spinal cord compression, or spinal stenosis.
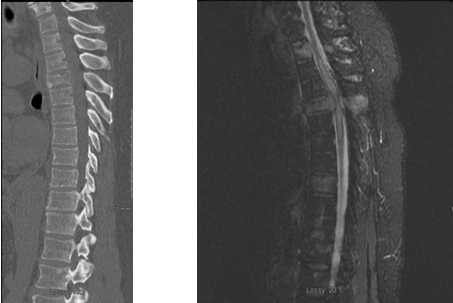
Upon physical examination, Dr. Frazier detected severe weakness in the patient’s legs and numbness from the patient’s mid-torso down to his feet. Suspecting metastatic spinal disease from prostate cancer, Dr. Frazier ordered x-rays and MRIs of the patient’s spine.
Preoperative imaging confirmed the following issues:
- Diffuse VCTs: As predicted, cancer from the patient’s prostate gland had spread to multiple vertebrae of the spine, including the mid-back, or thoracic spine.
- T4 Pathologic Fracture: As cancer invaded the bony tissues of the spine, the fourth thoracic vertebra (T4) had cracked from the pressure.
- Spinal Cord Compression: The abnormal cells (and shards of bone from the T4 fracture) were pressing against the patient’s spinal cord. This was causing symptoms of nerve dysfunction, such as muscle weakness, numbness, and a loss of bladder control.
- Myelomalacia: This condition occurs when an injury or obstruction (such as a spinal tumor) restricts blood flow to the spinal cord. Moreover, this disorder causes the spinal cord to soften, shrink, and become unstable. Evidence of a loss of spinal cord volume was present on the patient’s MRI.
After reviewing the patient’s x-rays, Dr. Frazier recommended the man for spine surgery.
Restoring Spinal Cord Function with Surgical Treatment
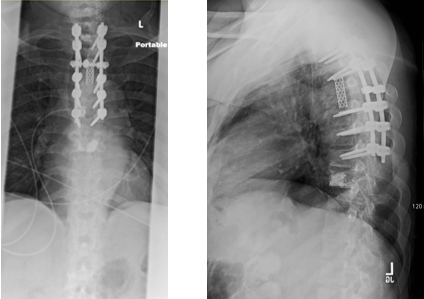
To restore function to the patient’s spinal cord, Dr. Frazier had to use a variety of surgical techniques. The first approach, known as a laminotomy, involved removing the back side of the affected vertebra. In our patient’s case, Dr. Frazier targeted the shattered vertebra at T4, as well as the nearby vertebrae at T3 and T5. (Unfortunately, the cancerous cells from the prostate gland had also migrated to these bones.)
The laminotomy was the “decompression phase” of the operation. During this stage, Dr. Frazier removed the laminae from T3-T5 to relieve strain on the spinal cord.
Following excision of the laminae, Dr. Frazier also removed the shattered vertebrae at T4, a technique known as a T4 transpedicular corpectomy. Pedicles are stout sections of bone that connect the vertebral body to the pointed tips that jut out from the back side of the vertebrae (aka, the processes). Transpedicular means that Dr. Frazier had to cut through each pedicle before he could remove the vertebral body, a procedure known as a corpectomy. (In Latin, the word corpus means body and -ectomy means to cut.)
After removing the burst vertebra, Dr. Frazier also detached the spinal tumor from the spine. To reinforce the spine (now devoid of a T4 vertebra), Dr. Frazier had to perform a posterior lumbar interbody fusion, or a PLIF. During the fusion process, Dr. Frazier inserted a bone graft into the interbody space and buttressed the spine using a mesh cage. After the surgery, the bone graft would continue to mature, fusing T3 and T5 into one strip of continuous and sturdy bone.
Lastly, Dr. Frazier performed a kyphoplasty to repair T3 and T5. Dr. Frazier injected medical-grade cement into the damaged vertebrae to restore the height to each vertebra, thus concluding the operation.
Minimally Invasive Spine Surgery (MISS) in Action
There are many advantages to using MISS to treat spinal tumors and back problems in general. Our patient was able to enjoy the following benefits of MISS:
- Less Blood Loss, Trauma, & Scarring: MISS is aptly named because it involves minimal trauma to the tissues that support our spine. In our patient’s case, Dr. Frazier was able to perform the entire operation using posterior entry only. This meant fewer (and smaller) incisions for our patient and only 650 cc of blood loss, or less than 3 cups. Several years ago, both of these feats–especially for a procedure of this magnitude–were unheard of.
- Shorter Procedures & Less Hospital Time: Dr. Frazier completed all aspects of this procedure in less than 4.5 hours of operative time. The patient (who had undergone 4 different procedures in 1) was able to return home in only 5 days.
- Quicker Recovery Rates: Less soft tissue dissection allowed our patient to start radiation and chemotherapy as soon as possible following his procedure. This was key to the patient’s ultimate recovery, as the underlying issue–prostate cancer–required further treatment options.
- Fewer Complications: In a patient with these traits (i.e. metastatic prostate cancer), MISS minimizes the risk of complications, such as post-surgical infections or slow-healing wounds.
Interested in learning about how MISS can help you? Dr. Frazier is a board-certified orthopedic spine surgeon with over 20 years of surgical experience in resolving spinal cord compression and vertebral column tumors. If you suffer from metastatic spine cancer, then contact Dr. Daveed Frazier, Harvard-trained spine surgeon today!