Case Study: Surgical Repair of L1 & L2 Burst Fractures

Meet the Patient
 The patient was a 51-year-old male, who had a history of alcoholism. The man had collapsed while having a seizure and found himself unable to walk after his fall.
The patient was a 51-year-old male, who had a history of alcoholism. The man had collapsed while having a seizure and found himself unable to walk after his fall.
When Dr. Daveed Frazier, spine surgeon, examined the patient’s lumbar spine, the man reported experiencing severe pain. It was this lower back pain–coupled with leg weakness–that were making it impossible for the patient to walk.
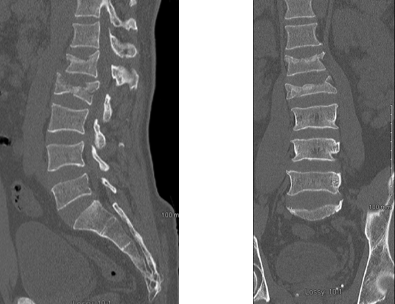
Dr. Frazier ordered X-rays of the patient’s lumbar spine, which revealed spinal fractures at the first and second lumbar vertebrae (known as L1 and L2). The vertebra at L1 had suffered from a compression fracture, meaning that the vertebra had caved in on its front side. At L2, the situation was even more dire. All four sides of the vertebra had shattered from the force of the fall.
In addition, the splinters of bone from the burst fracture at L2 had entered into the spinal canal, causing central canal stenosis. (This occurs when an obstruction in the spinal canal results in compression of the spinal cord and symptoms such as the patient’s leg weakness.)
Because of the compression fracture at L1, the lower back had lost some of the gentle inward sway (known as lordosis) that characterizes a healthy spine. Instead, the top of the lumbar spine arched forward (known as kyphosis). A form of traumatic (or injury-related) spinal deformity, these subtle changes in spinal curvature at L1 and L2 had knocked the entire spine out of alignment.
More Background Details: What is a Burst Fracture?
A burst fracture occurs when an extreme, vertical jolt causes a vertebra to shatter or “burst” upon impact.
The vertebrae of your spine stack up on one another to create a supportive pillar. (In fact, doctors often refer to the spine as the “vertebral column.”) Because the bones of your spine work as a team, each vertebra must withstand a tiny bit of compression from its neighbors. (In this case, compression means a squeezing force from above and below.)
Sudden events, like car accidents or falls, can ratchet this level of compression WAY up. If the squeezing force becomes too great, then even a healthy vertebra will shatter.
When a vertebra “bursts,” it shatters on all four sides. This is one of the most dangerous types of spinal fractures, because those tiny shards of bone can penetrate the spinal canal and wreak havoc. Namely, a spinal cord injury (SCI) can occur.
Although our patient did not suffer from an SCI with paralysis, his crushed vertebra was pinching his spinal cord. And, any form of canal compromise will affect how the body functions in the wake of an injury. As such, patients with burst fractures often report severe back or leg pain, difficulty walking, or neurological deficits such as muscle spasms or weakness.
Similarly, a compression fracture occurs when the front part of a vertebra collapses. This results in a wedge-shaped vertebral body that pitches the spine forward, out of alignment. Unfortunately, the end result of this is often kyphosis, or forward hunching of the spine.
Repairing the Vertebrae
 To repair the shattered vertebrae at L2, Dr. Frazier performed an XLIF Corpectomy.
To repair the shattered vertebrae at L2, Dr. Frazier performed an XLIF Corpectomy.
During the procedure, Dr. Frazier accessed the spine from the lateral side, using a tubular retractor. Performing the entire procedure through a metal tube allowed Dr. Frazier to minimize any trauma to surrounding structures, like the spinal cord. In addition, Dr. Frazier used live x-ray imaging to visualize the delicate tissues of the spine.
Next, Dr. Frazier removed the damaged discs above and below the level of the L2 burst fracture. The vertebral body of the shattered vertebra was then removed in a process known as a corpectomy. (The latin root of corp- means body, as in vertebral body, and -ectomy means to cut.)
After Dr. Frazier removed the vertebral body, an implant was inserted into the vacant space to reinforce the spine.
In addition, Dr. Frazier repaired the compression fracture at L1 by means of a kyphoplasty. During this procedure, Dr. Frazier filled the collapsed vertebra with a medical-grade cement, known as PMMA.
After Dr. Frazier had restored the height of each collapsed vertebrae, he added an expandable cage to the site of the corpectomy. Using a flexible and supportive cage allowed Dr. Frazier to avoid fusing the patient’s vertebrae together by means of a spinal fusion. In this manner, Dr. Frazier was able to preserve the patient’s range of motion in the lumbar spine.
Minimally Invasive Spine Surgery (MISS) in Action
Minimally invasive spine surgery (MISS) refers to any surgical technique that minimizes the patient’s exposure to trauma. Needless to say, MISS offers many benefits to the patient. In the case of our patient with L1 and L2 burst fractures, these gains included:
- Less Blood Loss, Trauma, & Scarring: Throughout the course of the procedure, the patient lost only 100 cc of blood. (This amounts to less than ½ a cup of blood loss.) Accessing the patient’s spine from the side and using tubular retractors allowed Dr. Frazier to preserve the strong muscles of the patient’s lower back. In other words, Dr. Frazier was able to keep tissue destruction down to a minimum.
- Less Operative Time: Dr. Frazier was able to perform this entire procedure in just under 4 hours.
- Less Postoperative Pain: In the days that followed the operation, the patient reported that his postoperative pain was minimal.
- Quicker Recovery Times: The patient was able to walk (or ambulate) on the first day after his surgery.
- Better Results: In a patient with a history of alcohol addiction and seizure disorders, MISS decreased the patient’s risk of spinal infection. In addition, Dr. Frazier was able to:
- Preserve the patient’s back muscles
- Restore the patient’s spinal alignment
- Reverse the patient’s kyphosis
To find out how minimally invasive spine surgery can help you too, contact our spine experts in Morristown, NJ and New York, NY today! Our Harvard-trained spine surgeon, Dr. Frazier, specializes in MISS for spinal injuries, unstable fractures, spinal deformities–and more!